Like billing to a private third-party payer, billers must send claims to Medicare and Medicaid. These claims are very similar to the claims you’d send to a private third-party payer, with a few notable exceptions.
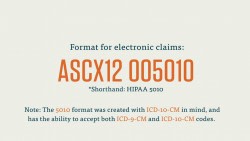
Since these two government programs are high-volume payers, billers send claims directly to Medicare and Medicaid. That means billers do not need to go through a clearinghouse for these claims, and it also means that the onus for “clean” claims is on the biller.
Billing for Medicare
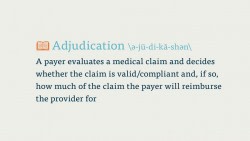
Before we get into specifics with Medicare, here’s a quick note on the administrative process involved. When a claim is sent to Medicare, it’s processed by a Medicare Administrative Contractor (MAC). The MAC evaluates (or adjudicates) each claim sent to Medicare, and processes the claim. This process usually takes around 30 days.
When billing for traditional Medicare (Parts A and B), billers will follow the same protocol as for private, third-party payers, and input patient information, NPI numbers, procedure codes, diagnosis codes, price, and Place of Service codes. We can get almost all of this information from the superbill, which comes from the medical coder.
If a biller has to use manual forms to bill Medicare, a few complications can arise. For instance, billing for Part A requires a UB-04 form (which is also known as a CMS-1450). Part B, on the other hand, requires a CMS-1500. For the most part, however, billers will enter the proper information into a software program and then use that program to transfer the claim to Medicare directly.
Parts C and D, however, are more complicated. Because Part C is actually a private insurance plan paid for, in part, by the federal government, billers are not allowed to bill Medicare for services delivered to a patient who has Part C coverage.
Only those providers who are licensed to bill for Part D may bill Medicare for vaccines or prescription drugs provided under Part D. If the provider is not a licensed Part D provider, the biller must assign that total directly to the patient (or the patient’s secondary insurance, if they have it, and if it covers that procedure or prescription).
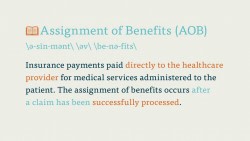
When a Part A claim is processed by Medicare, Medicare pays the provider directly for the service rendered by the provider. On the other hand, in a Part B claim, who pays depends on who has accepted the assignment of the claim. If the provider accepts the assignment of the claim, Medicare pays the provider 80% of the cost of the procedure, and the remaining 20% of the cost is passed on to the patient. You should recognized that 80-20 breakdown: it’s a classic example of coinsurance.
In certain cases, the provider will decline the assignment of the claim, and Medicare will assign payment directly to the patient. In cases like this, the patient, as opposed to the payer, must reimburse the provider for their services.
You should be aware, as well, that Parts A and B of Medicare have monthly and annual premiums, in addition to coinsurance arrangements depending on what kind of service the patient receives. These deductibles, premiums, co-pays, and coinsurance rates are fixed by CMS, but they can vary greatly between patients and procedures. Part of the challenge of filing a claim with Medicare is getting the proper number for each patient.
Billing for Medicaid
Creating claims for Medicaid can be even more difficult than creating claims for Medicare. Because Medicaid varies state-by-state, so do its regulations and billing requirements. As such, the claim forms and formats the biller must use will change by state. It’s up to the biller to check with their state’s Medicaid program to learn what forms and protocols the state follows.
In general, the medical biller creates claims like they would for Part A or B of Medicare or for a private, third-party payer. The claim must contain the proper information about the place of service, the NPI, the procedures performed and the diagnoses listed. The claim must also, of course, list the price of the procedures.
Be aware when billing for Medicaid that many Medicaid programs cover a larger number of medical services than Medicare, which means that the program has fewer exceptions.
One final note: Medicaid is the last payer to be billed for a service. That is, if a payer has an insurance plan, that plan should be billed before Medicaid.
In general, it’s much too difficult to describe the full process of billing Medicaid without going into an in-depth description of specific state programs. As this is just a basic introductory course, we won’t go into much more depth than this.