In the previous course, we introduced you to HIPAA. In this course, we’ll show you how it affects the practice of medical billing.
Whether you know it or not, you’re actually already familiar with many of the provisions laid out by HIPAA. One of the most readily felt impacts of HIPAA is the standardization of medical codes used by coders and billers.
As we discussed in the last Course, HIPAA formalized the use of ICD codes for diagnosis and CPT and HCPCS codes for procedural reporting. We use these codes every day in medical billing to create claims.
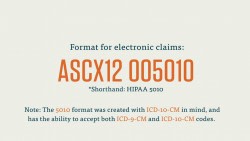
HIPAA establishes and manages electronic medical transactions. Title II of HIPAA requires all providers and billers covered by HIPAA to submit claims electronically using the approved format. This format is known as ASC X12 005010. You may encounter the shorthand for this form as “HIPAA 5010.”
It’s important to remember that HIPAA 5010 does not necessarily prescribe the format of a claim, so much as the way it is transferred. You can think of HIPAA 5010 transactions as vehicles with uniform exteriors. They all must look the same, but each vehicle might carry different passengers in different arrangements (in this case, medical information).
Within ASC X12 005010, each type of transaction gets its own code set number. Let’s look at these code set numbers, and the type of transactions they correspond to, now. You’ll see that each code set number is preceded by an “X12.” This is to remind you that the code set is monitored and maintained by the ASC X12. Each of these transactions takes the form of a particular Electronic Data Interchange (EDI).
Each of these types of transaction forms has their own rules and formats. For simplicity’s sake, we’ve focused on the health care claim (the first code set number listed below), and we’ll continue to do so for the rest of the courses. The additional forms, and their code set numbers, are listed for your general knowledge in the downloadable ebook.
HIPAA Forms and Their Code Set Numbers
Health Care Claim Transaction
- Code set number: X12 837
- The health care claim is the most basic and common type of electronic medical transaction. Billers use claims to request reimbursement on the behalf of providers. Claims include information about the patient, the provider, the patient’s health insurance plan, in addition to codes for the procedure and diagnosis.
Just as medical coders have to use the appropriate code set to describe a procedure or diagnosis, so too do medical billers have to use the right type of EDI to perform a certain billing task.
As you can see, HIPAA’s impact extends to almost every aspect of the medical billing process, from how records are stored and accessed to how codes are used in creating claims. As you pursue your formal training in medical billing, you’ll learn even more about HIPAA and the ways its affects medical billing.