In the past, coders entered their codes into paper forms, which they then passed on to the medical billing individual or organization. Today, in order to speed up the coding process and ensure more accuracy, the majority of the medical coding profession uses some type of coding software.
Software programs like Epic, Centricity, AdvancedMD, Flash Code, Eclipse, and others have fields where coders can enter the correct procedure and diagnosis codes. These software programs may come with look-up tools that help coders find the correct code, but coders should always use their coding manuals to get the last word on which codes to use.
Epic is considered by many to be the gold standard and one of the more complicated programs. Coders who familiarize themselves with the Epic software program should be well suited to mastering other coding programs. These programs are often paired with medical billing programs.
Because these programs are copyrighted, and because using them requires a more complete understanding of the coding process and its day-to-day requirements, we won’t be covering them in great depth in this course. Instead, we’ll look at some of the things you’ll be able to do with coding software.
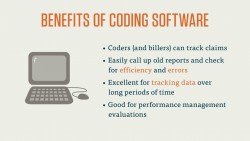
The benefits of working with coding software are numerous. Coders (and billers) can track claims and easily call up old reports to check for efficiency and errors. Coding software is also excellent for tracking data over long periods of time and for performance management evaluations. Software like Epic and Eclipse can help coders keep track of their lag time for codes, allowing for better organization and a faster turnaround in the reimbursement cycle. Many coding programs also check, automatically, for compatible codes, though the onus is always on the coder to check and double-check using their coding manuals.
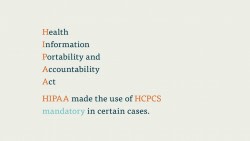
A good coding software program should meet the needs of your practice or coding organization. Coding software should also be compliant with CMS-1500 forms and all HIPAA regulations (we’ll cover both of these in Courses 3-4 and 3-8, respectively). Put simply, CMS-1500 is the general form used to send claims to Medicare, Medicaid, and many other third-party payers, and HIPAA is a law that created a set of standards for electronic billing and coding in the mid-1990s.
Bear in mind that most coders won’t get to select the software they use, unless they start their own coding business. That usually doesn’t happen until a coder has five to ten years of professional experience.