By now, you should have a decent grasp on the basics of the medical coding practice. Before we wrap up the section with a quiz, you can use this course to review some of the basic information we’ve covered.
Let’s begin the review.
International Classification of Diseases, Tenth Revision, Clinical Modification (ICD-10-CM)
Published by the World Health Organization (WHO) in 1999 and implemented in the U.S. in 2015, ICD-10-CM contains more than 141,000 codes to report healthcare diagnoses and procedures. ICD-10-CM is three to seven characters long, and is entirely alphanumeric. The system is organized into “chapters” or sections based on the type of disease or condition shown in the diagnosis.
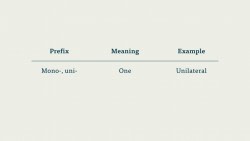
ICD-10-CM codes all have three-character categories and one-digit subcategories. The subcategory follows the decimal point after the category. ICD-10-CM codes feature up to three subclassifications. These extra subclassifications allow ICD-10-CM to feature specific information about the disease or injury described in the diagnosis. ICD-10-CM, for example, has codes for laterality—which side of the body the injury or illness is on.
ICD-10-CM codes also feature alphabetic extensions. These extensions can only occupy the seventh and final character of an ICD-10-CM code, and describe the episode of care for the injury or illness. In other words, extensions show which visit this is for a particular condition. These may be broadly divided into categories of “initial encounter” (the first visit for a condition), “subsequent encounter” (A follow-up for the same condition), or “sequela” (a visit for a condition stemming from a prior condition).
Extensions are typically used in codes for Injury and codes for Childbirth, though they may show up elsewhere. In the case of adding an extension to a code that does not go to the final subclassification, codes use placeholders, typically the letter X.
Crosswalking
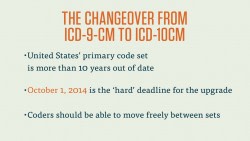
Before ICD-10-CM was implemented in the U.S. on October 1, 2015, healthcare venues across the nation were using the ICD-9-CM system. The transition was made because ICD-10-CM has more “room” for new codes, and its focus on specific iterations of certain conditions make it a far more data-rich code set for health organizations, health providers, and insurance companies. Additionally, the rest of the world was at that point already using some version of ICD-10-CM.
While ICD-9-CM is no longer actively used in the U.S., coders may still need to translate codes back and forth from one set to the other.
We transfer between newer and older versions of coding systems through a process called crosswalking. Crosswalking entails the mapping of similar information across similar but distinct data sets. You could think of translating between two languages as a sort of crosswalking: ‘bread’ in English is ‘pan’ in Spanish.
You can crosswalk between any two code sets, but for the sake of simplicity we’ll confine it to ICD-9-CM and ICD-10-CM.
Crosswalking entails finding exact, approximate, or appropriate matches between the two code sets. Since there are far more codes in ICD-10-CM than ICD-9-CM, it’s generally much easier to find an appropriate match for an ICD-9-CM code in ICD-10-CM than the other way around. We call the code in the first set the “source,” and the code to which we’ll match the source the “target.” When crosswalking, you may go from the specific to the general, but you may never infer specific information from a general diagnosis. That is, you could crosswalk a diagnosis of “closed fracture of distal phalanx of great toe on left foot” to “fracture of distal phalanx of great toe,” but you could never crosswalk those diagnosis codes in the opposite direction.
Crosswalking is not an exact science. Less than a quarter of ICD-10-CM codes have exact matches in ICD-9-CM. The goal of crosswalking is to facilitate the transfer between these two code sets and allow better data tracking. In order to assist coders, the National Center for Health Statistics (NCHS) has created a set of General Equivalency Mappings (GEMs). These list appropriate matches between the two code sets, and are invaluable resources as you move further in crosswalking.
Current Procedure Terminology (CPT)
ICD codes describe the why of a medical procedure. CPT codes describe the what. CPT codes correspond to almost every medical procedure performed by a healthcare provider, and are the primary way that providers inform payers of their services.
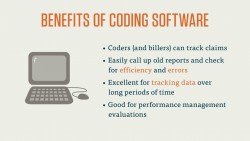
CPT codes are divided into three Categories. These Categories are different than the categories in ICD, of course. CPT Categories refer to the division of the CPT code manual: Category I is the larger and more important Category. Category I contains the codes for procedures in the six major fields of health care. Category II contains supplementary codes that may be used to add or track data, and are often used in performance management.
Category I CPT codes are five digits long and entirely numeric. (Category II is alphanumeric, but we’ll focus our attention on Category I here). Category I is divided into six sections, each corresponding to a major field of medicine. The sections are: Evaluation and Management, Anesthesiology, Surgery, Radiology, Pathology and Laboratory, and Medicine. These sections are, for the most part, ordered numerically. (Evaluation and Management is out of order and placed at the front Category I for ease of access—E&M codes are used frequently by most practices).
Each section in Category I is broken down into further subsections. For example, the Surgery section is subdivided into sections based on where on the body the surgery is performed. Those subsections are then further divided by what kind of surgical procedure (an incision vs. an excision, for example) is being performed.
Many Category I CPT codes are procedures that are based on a general, “parent” procedure. The parent procedure is often a basic or simplified version of the procedure, while the codes indented below it describe variations on that procedure that are too specific to be included in the parent code.
Let’s look briefly at Category II and III codes. Category II codes are optional codes that are added to Category I or Category III codes. Category II codes describe things like patient management, patient history, and the results of certain diagnostic or screening tests. Category II codes are supplemental and may never take the place of a Category I or Category III code.
Category III contains temporary codes for emerging and experimental procedures. CPT is updated annual to keep up with new and emerging medical procedures and technologies, and Category III is the place where new procedures go for their “test run.” Before a procedure can be added to Category I, it needs to be performed a certain number of times by a certain number of different providers. Category III is where the codes that are not yet official, but are being tested out, reside.
CPT Modifiers
CPT modifiers are an important part of coding with CPT. These two-digit, entirely numeric modifiers are added to the end of a CPT code with a hyphen, and may describe the what, the who, the where, and the how of a particular procedure. There are modifiers for things like multiple surgeons, discontinued procedures, and increased procedural services. These modifiers are integral in the reimbursement cycle, as they tell the payer that a provider had to work more (or less) during a particular procedure.
Because these modifiers can be very important to the billing process, we order them in such a way that the most important, or “functional” modifier goes first. That is, if there is a modifier for “increased procedural services” (-22) and one for “bilateral procedure” (-50) we’d code the -22 modifier first, as it tells the payer that the provider had to perform extra work.
The reason for this is simple: despite the fact that most claims have room for up to four modifiers for each procedure, many third party payers sometimes ignore modifiers after the first two. For this reason, it’s important the modifiers directly related to the reimbursement cycle come first.
Healthcare Common Procedure Coding System (HCPCS)
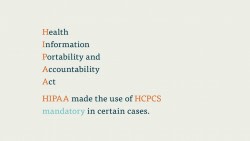
The final of the three critical code sets used by medical coders is HCPCS (pronounced hick-picks). Developed by the Center for Medicare and Medicaid Services (CMS), HCPCS is the primary way that billers describe procedures to Medicare, Medicaid, and a host of other third-party payers.
HCPCS is based on CPT. So much so that the first section (Level) of HCPCS is identical to CPT. It’s a bit technical, but when you use CPT, but submit it to Medicare, Medicaid, or one of the third-party payers that accepts HCPCS, those CPT codes become HCPCS codes. You don’t have to enter anything differently. Since the code sets are the same, payers simply recognize Category I CPT codes and Level I HCPCS codes as interchangeable.
The code sets diverge with HCPCS Level II. HCPCS Level II describe the various non-physician services administered or prescribed by healthcare providers that aren’t covered in CPT. It’s a broad swath of codes—so broad that HCPCS is sometimes referred to as the “hall closet of medical coding.” It’s got a little bit of everything in there.
These codes are five characters long and alphanumeric. The code set is divided by area of focus and assigned a letter, which doubles as the first character of the code. For instance, B-codes are for Enteral and Parenteral Therapy, E-codes are Durable Medical Equipment, P-codes are Pathology and Laboratory, and so on. Level II Codes include dosages of non-orally administered medicine (like injections) and each specific type of splint, so the code is extremely specific.
Coders use HCPCS Level II just as they would CPT. If there is equipment, certain professional services, injected medication, or any number of things listed on the report that aren’t found in CPT, the coder should use HCPCS Level II.
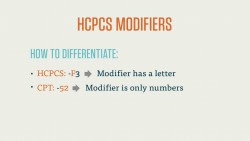
HCPCS Modifiers
Like CPT, HCPCS has a set of two-character modifiers that provide important additional information about the code. These modifiers are added to the end of either CPT or HCPCS Level II codes with a hyphen. You may use HCPCS modifiers alongside CPT codes and CPT modifiers. You can tell whether a modifier is a HCPCS or CPT modifier quite easily: CPT modifiers are always numeric, and HCPCS modifiers are always alphanumeric.
There are significantly more HCPCS modifiers than CPT modifiers. HCPCS modifiers may describe everything from the type of ambulance service performed to the location on the body a procedure was performed.
Bear in mind that certain HCPCS modifiers do not “agree” with certain CPT modifiers. The most common of these mutually exclusive relationships is the HCPCS modifiers –LT and –RT, which describe which side of the body a procedure is performed on, and the CPT modifier -50, which describes a bilateral procedure. Obviously something can’t be performed on the left side of the body and be a bilateral procedure.
As with CPT modifiers, coders should always order functional HCPCS modifiers first, and informational modifiers second.
That concludes our review. Before taking the review quiz, feel free to rewatch any course videos and look at our downloadable materials for extra information.