Like medical coding, the profession of medical billing has its own specific vocabulary. In this course, you’ll learn about some of the key terms and concepts in the medical billing field. We’ll expand on a number of these topics in later courses. For a fuller list of medical billing vocabulary, download our ebook.
Allowed Amount
The amount an insurance company will pay to reimburse a healthcare service or procedure. The patient will typically pay the balance if there is any remainder.
Appeal
The process by which a patient or provider attempts to persuade an insurance payer to pay for more (or, in certain cases, pay for any) of a medical claim. The appeal on a claim only occurs after a claim has either been denied or rejected (See “Rejected Claim” and “Denied Claim”).
Applied to Deductible (ATD)
The amount of money a patient owes a healthcare provider that goes to paying their annual deductible (See “Deductible”). A patient’s deductible varies, and depends on that patient’s insurance policy.
Assignment of Benefits (AOB)
Insurance payments paid directly to the healthcare provider for medical services administered to the patient. The assignment of benefits occurs after a claim has been successfully process.
Capitation
An arrangement between a healthcare provider and an insurance payer that pays the provider a fixed sum for every patient they take on. Capitated arrangements typically occur within HMOs (See “Health Maintenance Organization (HMO)”). HMOs enlist patients to service providers, who are paid a certain amount based on the patient’s health risks, age, history, race, etc.
Clean Claim
A claim received by an insurance payer that is free from errors and processed is a timely manner. Clean claims are a huge boon to providers, as they reduce turnaround time for the reimbursement process and lower the need for time-consuming appeals processes. Many providers send their claims to third parties, like clearinghouses (See “Clearinghouse”), that specialize in creating clean claims.
Clearinghouse
A third-party organization in the billing process, and separate from the healthcare provider and the insurance payer. Clearinghouses review, edit, and format claims before sending them to insurance payers. This process is sometimes called “scrubbing.”
Centers for Medicare and Medicaid Services (CMS)
A federal agency that manages and oversees healthcare coverage through Medicare and Medicaid. CMS, if you remember from Section 2, also maintains HCPCS codes. CMS directly affects the healthcare of over 100 million Americans, and this number is growing every day. (See “Medicare” and “Medicaid”).
CMS 1500
A paper form used to submit medical claims to Medicare and Medicaid. Many commercial insurance payers also require providers to submit their claims using a CMS 1500, making this one of the most common and important tools in the medical billing process.
COBRA Insurance
A federal program that grants a person recently terminated to retain health insurance with their former employer for 18 months, and up to three years if the former employee is disabled.
Co-insurance
A type of insurance arrangement between the payer and the patient that divides the payment for medical services by percentage. While this is sometimes used synonymously with a co-pay, the arrangements are different: While a co-pay is a fixed amount the patient owes, in a co-insurance, the patient owes a fixed percentage of the bill. These percentages are always listed with the payer’s percentage first (eg a 70-30 co-insurance).
Explanation of Benefits (EOB)
A document attached to a processed claim that explains to the provider and patient which services an insurance company will cover. EOBs may also explain what is wrong when a claim is denied.
Electronic Remittance Advice (ERA)
A digital version of the EOB, this document describes how much of a claim the insurance company will pay and, in the case of a denied claim, explains why the claim was returned.
Fiscal Intermediary (FI)
A Medicare representative who processes Medicare claims.
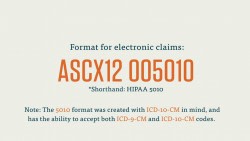
Health Insurance Portability and Accountability Act (HIPAA)
A law passed in 1996 that has lasting effects on the healthcare industry today. Title I of the act protects workers’ health insurance when they change or lose jobs. Title II of the Act established standards and best practices in electronic health care. Refer to Courses 3-8 and 3-9.
Health Maintenance Organization (HMO)
A network of healthcare providers that offer coverage to patients for medical services exclusively within that network. We’ll cover this type of insurance more thoroughly in later videos.
Independent Practice Association (IPA)
A professional organization of physicians or healthcare providers who have a contract with an HMO. HMOs contract IPAs to provide services to patients within the HMO’s network, but their individual practices do not have to be part of the HMO network.
Managed Care Plan
A type of insurance plan wherein patients are only eligible to receive health care within the insurance company’s network. HMOs and IPAS (See “Health Maintenance Organization (HMO)” and “Independent Practice Association (IPA)”) are examples of the managed care system.
Medicare
A government insurance program, founded in 1965, that provides healthcare coverage for persons over 65 years old and for people with disabilties. Medicare provides coverage to more than 50 million people in the United States today, and is one of common places you’ll send your medical claims to.
Medicaid
Medicaid provides insurance coverage to low-income families and individuals. It is essentially an insurance program for those who cannot afford full insurance coverage. Medicaid is funded at state and federal levels, but each state has it’s own version of Medicaid that must operate above the minimum requirements established by federal law.
Point of Service (POS) Plan
In this insurance plan, a patient in an HMO network can go to a physician outside of their network if they are referred there and pay a higher deductible. Think of this as a cross between an HMO and basic indemnity insurance (See “Health Maintenance Organization” and “Indemnity”).
Preferred Provider Organization (PPO)
A plan similar to an HMO, except that the insurance company, rather than the HMO itself, decides who is in the acceptable provider network. This is a common, subscription-based type of managed care.
Triple Option Plan (TOP)
Sometimes called a “cafeteria plan,” this plan provides individuals who sign up the option of choosing between an HMO, PPO, or POS coverage (See “Health Maintenance Organization (HMO),” “Preferred Provider Organization (PPO),” and “Point of Service (POS) Plan”).
TRICARE
Formerly known as CHAMPUS, this is a federal health insurance plan for active service members, retired service members, and their families.
UB04
Similar in format to the CMS 1500 (See “CMS 1500”), this is another one of the most common claim forms.
Utilization Limit
Medicare places a yearly limit on certain medical services. If a patient passes this threshold, known as the utilization limit, they may be ineligible for Medicare coverage for that procedure.